Hard Tissue Bonding in Dentistry: A Comprehensive Overview
Hard tissue bonding is a cornerstone of modern dentistry, revolutionizing restorative, cosmetic, and preventative treatments. It involves adhering restorative materials (like composites, ceramics, and metals) to tooth structure (enamel and dentin) using adhesive systems. Here’s a detailed breakdown covering the principles, materials, techniques, clinical applications, advantages, disadvantages, and future trends:
I. Principles of Hard Tissue Bonding
The success of hard tissue bonding relies on achieving a strong, durable, and biocompatible interface between the restorative material and the tooth. This involves several key steps:
- Etching: Creating micro-porosity on the enamel and dentin surface to increase surface area for bonding. This is typically achieved using acids (phosphoric acid, hydrofluoric acid).
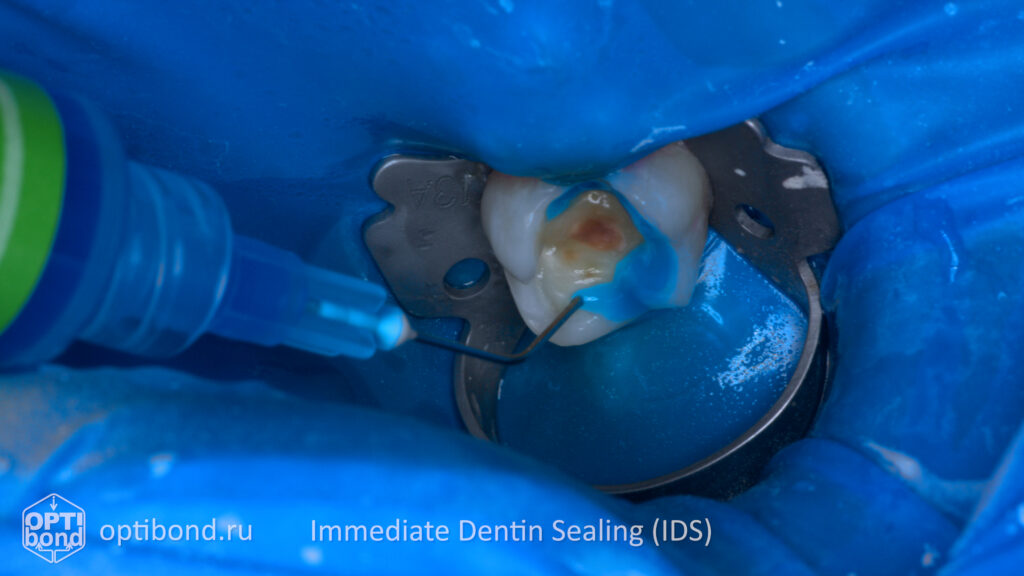
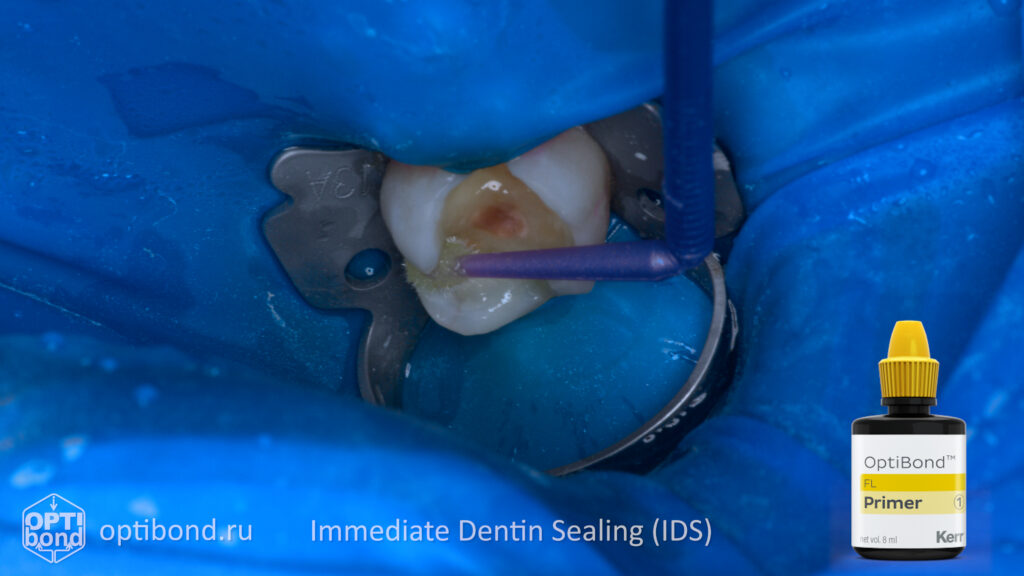
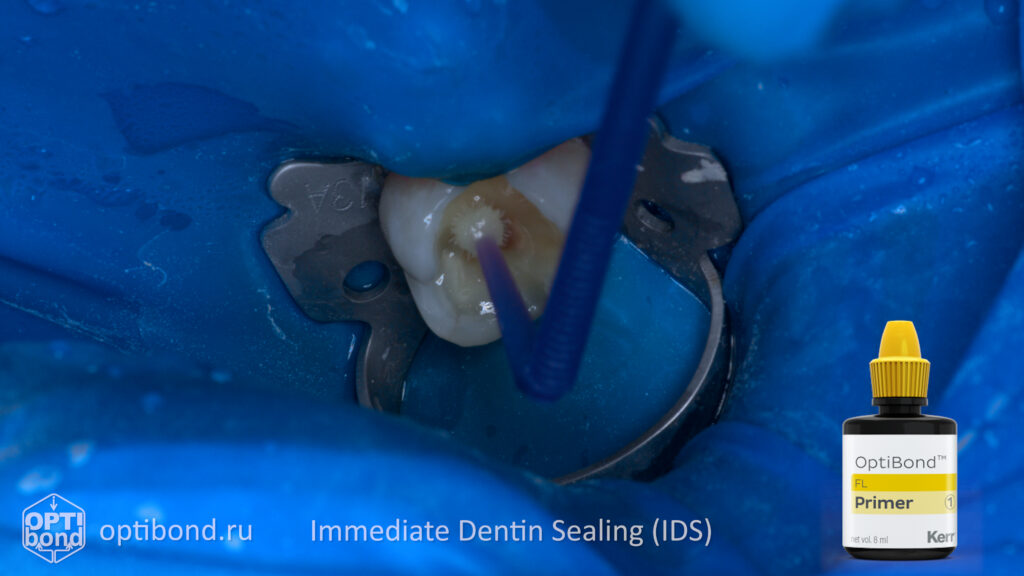
- Priming: Applying a primer to the etched surface to improve wetting of the adhesive and to create a hybrid layer. Primers contain monomers that infiltrate the etched surface and chemically bond to both the tooth structure and the restorative material.
- Bonding: Applying an adhesive resin (bonding agent) that penetrates the hybrid layer and polymerizes, creating a chemical and mechanical bond between the tooth and the restoration.
Key Factors Influencing Bond Strength:
- Surface Preparation: Proper etching and priming are crucial.
- Moisture Control: Contamination with saliva or blood drastically weakens bond strength.
- Adhesive System Chemistry: Different adhesives have varying properties and bond strengths.
- Restorative Material: The type of material being bonded influences the adhesive chosen.
- Polymerization: Complete polymerization of the adhesive is essential for optimal strength.
- Clinical Technique: Operator skill and adherence to protocols are vital.
II. Materials Used in Hard Tissue Bonding
- Etchants:
- Phosphoric Acid (30-37%): Commonly used for enamel etching. Creates a microporous surface.
- Hydrofluoric Acid (9.6%): Used for etching porcelain and glass ceramics.
- Self-etching Primers/Adhesives: Combine etching and priming steps, simplifying the process.
- Primers:
- HEDP (Hydroxyethyl Methacrylate): Improves wetting and bond to dentin.
- 4-META (4-Methacryloxyethyl Trimellitic Anhydride): Enhances bond to enamel.
- Adhesive Resins (Bonding Agents):
- Traditional 3-Step Systems: Etch, Prime, Bond (separate steps).
- 2-Step Systems: Combine Prime and Bond.
- 1-Step (Self-Etch) Systems: Combine etching, priming, and bonding.
- Universal Adhesives: Designed to bond to a wide range of materials (enamel, dentin, zirconia, metal) with minimal technique sensitivity.
- Restorative Materials:
- Composite Resins: Most commonly bonded material.
- Ceramics (Porcelain, Lithium Disilicate, Zirconia): Bonded using resin cements.
- Metals (Gold, Alloys): Bonded using resin cements or mechanical retention.
III. Bonding Techniques
- Total-Etch Technique:
- Enamel and dentin are etched with phosphoric acid.
- Etched surface is rinsed and dried.
- Primer is applied and allowed to penetrate the dentin.
- Adhesive resin is applied and polymerized.
- Self-Etch Technique:
- Self-etching primer/adhesive is applied to the tooth surface.
- The acid component etches the enamel and dentin simultaneously while the monomers penetrate.
- Adhesive resin is applied and polymerized.
- Selective Etch Technique: Etching only the enamel, leaving the dentin protected. Used for indirect restorations to preserve the dentin structure.
- Universal Bonding: Using a universal adhesive system that can bond to both enamel and dentin with minimal technique sensitivity.
IV. Clinical Applications of Hard Tissue Bonding
- Direct Restorations: Composite fillings (Class I-VI restorations).
- Indirect Restorations: Bonding porcelain inlays, onlays, crowns, veneers, and bridges.
- Tooth-Colored Laminates (Veneers): Enhancing aesthetics.
- Orthodontic Bonding: Attaching brackets to teeth.
- Pit and Fissure Sealants: Preventing caries.
- Repair of Restorations: Bonding composite to existing restorations.
- Root Canal Sealant Bonding: Securing core build-ups.
- All-Ceramic Restorations: Bonding lithium disilicate and zirconia restorations.
- Periodontal Splinting: Stabilizing mobile teeth.
V. Advantages of Hard Tissue Bonding
- Tooth Conservation: Minimizes removal of healthy tooth structure.
- Aesthetics: Allows for tooth-colored restorations.
- Versatility: Can be used for a wide range of applications.
- Strength and Durability: Provides a strong and durable bond.
- Improved Marginal Adaptation: Reduces microleakage.
- Reduced Sensitivity: Bonding can seal dentinal tubules.
- Simplified Procedures: Some techniques are streamlined and less invasive.
VI. Disadvantages of Hard Tissue Bonding
- Technique Sensitivity: Proper technique is crucial for success.
- Moisture Control: Contamination can weaken bond strength.
- Postoperative Sensitivity: Can occur, especially with deep restorations.
- Polymerization Shrinkage: Can lead to stress and microleakage.
- Wear and Discoloration: Composite restorations can wear and stain over time.
- Bond Failure: Can occur due to improper technique, contamination, or material limitations.
VII. Future Trends in Hard Tissue Bonding
- Bioactive Adhesives: Adhesives that promote remineralization and reduce secondary caries.
- Self-Adhesive Materials: Materials that bond to tooth structure without etching or priming.
- Improved Polymerization Techniques: Light-curing units with optimized wavelengths and intensities.
- Nanotechnology: Incorporating nanoparticles into adhesives to enhance strength and durability.
- Smart Adhesives: Adhesives that release fluoride or antibacterial agents.
- Digital Dentistry Integration: CAD/CAM systems for precise restoration design and bonding procedures.
Conclusion:
Hard tissue bonding is an indispensable part of modern dentistry, offering numerous advantages over traditional restorative techniques. Ongoing research and development continue to improve adhesive materials and techniques, further enhancing the strength, durability, and biocompatibility of bonded restorations. A thorough understanding of bonding principles, proper technique, and material selection are essential for achieving predictable and long-lasting clinical results.
Reference:
- Dental Hard Tissues and Bonding Interfacial Phenomena and Related Properties – George Eliades, DDS, Dr.Dent. David Watts, PhD, DSc, FADM Theodore Eliades, DDS, MS, Dr.Med., PhD, FADM – ISBN-13 978-3-540-23408-1
- Management of Deep Carious Lesions – Editor Falk Schwendicke Department for Operative and Preventive Dentistry – ISBN 978-3-319-61369-7
- Dental Caries The Disease and Its Clinical Management Third Edition – Edited by Ole Fejerskov, Bente Nyvad, and Edwina Kidd – ISBN 978-1- 118-93582 -8
- Noncarious Cervical Lesions and Cervical Dentin Hypersensitivity: Etiology, Diagnosis, and Treatment Edited by Paulo V. Soares, DDS, MS, PhD John O. Grippo, DDS ISBN 9780867157543
- Pulp-Dentin Biology in Restorative Dentistry – Ivar A. Mjör, BDS, MSD, MS, Dr odont – ISBN 0-86715-412-8




